Attention-Deficit/Hyperactivity Disorder (ADHD), Trauma, and Neuropsychology: Exploring the Overlap
Introduction Attention-Deficit/Hyperactivity Disorder (ADHD) and experiences of trauma, particularly in childhood, exhibit notable overlaps in symptoms, leading to complexities in diagnosis and treatment. A neuropsychological perspective provides insight into these overlaps and underscores the importance of accurate assessment.
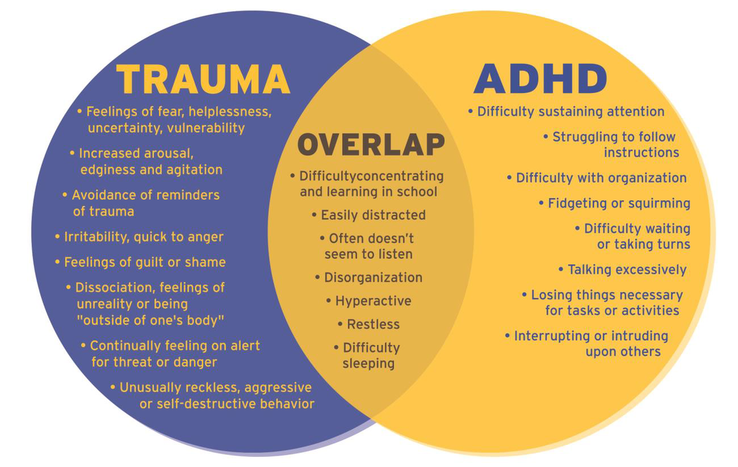
Neuropsychological Overlaps Between ADHD and Trauma Both ADHD and trauma can result in difficulties with attention, impulse control, and emotional regulation. Neuropsychological assessments, such as the Stroop Task and Trail Making Test, are employed to evaluate these cognitive functions. However, these tools may not effectively distinguish between ADHD and trauma-related impairments, as both conditions can similarly affect executive functioning.
Furthermore, individuals with ADHD may be at an increased risk for developing Post-Traumatic Stress Disorder (PTSD), suggesting a bidirectional relationship between the two conditions. This interplay complicates the clinical picture, making comprehensive evaluations essential.
The Link Between ADHD/ADD and Trauma ADHD and Attention-Deficit Disorder (ADD) are neurodevelopmental conditions characterized by symptoms such as inattention, hyperactivity, and impulsivity. Emerging research suggests a complex relationship between these disorders and experiences of trauma, particularly in childhood. Understanding this connection is crucial for accurate diagnosis and effective treatment.
Studies indicate that individuals who have experienced traumatic events may exhibit symptoms similar to those of ADHD or ADD. For instance, children exposed to trauma might display inattention, hyperactivity, and impulsivity—core symptoms of ADHD. This overlap can sometimes lead to misdiagnosis. The Child Mind Institute emphasizes that while ADHD is a brain development disorder, trauma responses can mimic its symptoms, making accurate diagnosis challenging.
Shared Symptoms and Diagnostic Challenges Both ADHD and trauma responses involve difficulties with concentration, restlessness, and emotional regulation. However, the underlying causes differ: ADHD is primarily a neurodevelopmental condition, whereas trauma responses are reactions to distressing events. WebMD notes that distinguishing between the two is essential, as the treatments differ significantly.
Impact of Childhood Trauma on ADHD Diagnosis Research suggests that children with a history of trauma may be more likely to receive an ADHD diagnosis. Medical News Today reports that negative memory bias associated with traumatic experiences can exacerbate symptoms like inattention and hyperactivity, potentially leading to misdiagnosis.
Adult ADHD and Trauma In adults, the interplay between ADHD and trauma can complicate diagnosis and treatment. WebMD highlights that adults with ADHD are more likely to have PTSD compared to those without ADHD. This comorbidity can intensify symptoms and hinder treatment efforts.
Hypnosis as a Complementary Treatment Approach Hypnotherapy has emerged as a potential complementary treatment for managing ADHD symptoms. By promoting deep relaxation and heightened focus, hypnosis may enhance self-regulation and concentration in individuals with ADHD. A study comparing cognitive-behavioural therapy (CBT) and hypnotherapy found that both treatments led to improvements, but the hypnotherapy group reported significantly better psychological well-being and reduced ADHD symptoms.
While hypnosis is not a replacement for traditional medical or psychological treatments, it can serve as a valuable adjunct. It works synergistically with other therapeutic approaches, such as CBT, mindfulness, and medication, by enhancing self-awareness and emotional resilience.
Importance of Accurate Diagnosis Given the symptom overlap, it is vital for clinicians to conduct comprehensive assessments that consider both ADHD and potential trauma histories. Misdiagnosis can lead to ineffective treatments; for example, stimulant medications for ADHD may not address underlying trauma and could potentially worsen anxiety symptoms. The Child Mind Institute advises that understanding a client’s full history is crucial to developing an effective treatment plan.
Conclusion The neuropsychological similarities between ADHD and trauma necessitate thorough assessments to ensure accurate diagnosis and effective treatment planning. Incorporating complementary therapies like hypnotherapy may offer additional benefits in managing ADHD symptoms, particularly when traditional treatments are insufficient. Awareness of the potential link between trauma and ADHD/ADD symptoms is essential for accurate diagnosis and effective intervention.